 The Relationship Between Chronic Pain, Leaky Gut Syndrome, and Depression
The Relationship Between Chronic Pain, Leaky Gut Syndrome, and Depression
Depression, coupled with chronic pain and leaky gut syndrome, is a common problem that I frequently see in my patients.
In fact, according to the Centers for Disease Control, 1 in 10 Americans is currently taking medication to treat depression. But before rushing to find a suitable naturopathic alternative, I prefer to stand back, listen, and try to determine why my patient is suffering from depression in the first place.
Sometimes the causes of depression are circumstantial—such as grief over the death of a loved one. Or, the cause may be due to past trauma, a chemical imbalance in the brain, poor daily habits, or genetics. And finally, we see depression in cases of chronic pain and disease. In the case of chronic pain, the disease process may have begun many years before and evolved slowly over time.
A Type Of Pain That Evolves Slowly
The problem with chronic pain is that, it may develop so slowly; that we are inclined to ignore it—like the proverbial frog in hot water. Consequently, the pain is pushed to the side so often; that a person may not seek medical attention until the disease process is quite advanced. And one of the ways in which chronic disease is expressed is lingering low-grade depression.
One of the most common types of chronic disease, associated with depression, concerns medical conditions that can have a negative impact on digestive health. This has often been referenced as the gut-brain connection and refers to the relationship between emotional well-being and digestive health.
Common Digestive Health Challenges Associated With Depression
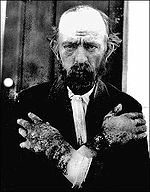
Common digestive health challenges, associated with chronic pain and depression, often start off as mild digestive complaints, like gas, bloating, acid reflux and upset stomach, but may evolve into severe unrelenting pain, accompanied by other symptoms like, acne, migraines, joint pain, fatigue and chronic low grade depression—as the disease process progresses.
Depression is a common side effect of disease and seems to have evolved as an adaptive response to stress.
The function of depression during times of ill health appears to be in the fact that illness encourages people to rest, and conserve energy—energy that can then be used to repair the body. A similar depression may occur during times of drought, famine, and wintertime—when food resources are limited.
Testing For Depression in a Clinical Setting
While no adequate testing yet exists to determine the physiological causes of depression, I do test my patient’s neurotransmitter levels with urine neurotransmitter metabolite testing from Labrix.
Neurotransmitter testing can be done from the convenience of your own home, with a self-collected urine sample. And can offer some basic information about brain health and brain function. Neurotransmitter profile testing looks at serotonin, dopamine, norepinephrine, epinephrine, glycine and histamine metabolite levels—the chemical messengers associated with mood.
While not a perfect test, I have been able to effectively treat depression, and determine appropriate supplementation, using urine metabolite testing.
Cleaning up the Diet in Cases of Depression
One of the first things I address, when treating depression, is the need to support optimal nutrition. This is especially true in individuals with maldigestion coupled with malabsorption.
When supporting good nutrition, I start with removing those foods associated with food allergies, sensitivities, and poor nutrition—foods like sugar, processed foods, gluten, and dairy. Gluten and dairy are almost always removed because they are associated with “leaky gut,”: a condition whereby the intestinal lining is damaged and weakened due to food sensitivities, allergies, infection, and or autoimmune conditions, like celiac disease.
Dairy and wheat also contain gluteomorphins and casomorphins—substances found in the digestive tracts of people who suffer from autism, schizophrenia, and depression, and thought to have a negative impact on mental health.
Consequently, they are removed in the early stages of treating most health challenges associated with depression. Remember, the chronic disease process almost always gives way to depression, and is almost always, at least partially, associated with poor digestion.
Additional foods that are associated with weak digestion and chronic depression include legumes like soy, commercial eggs, and commercial red meat.
When in Doubt, a Clean Diet Minimally Processed Is Prescribed
An ideal diet to encourage a positive mood, would include, plenty of fresh fruits and vegetables, whole grains, like quinoa, brown rice, kasha and millet, nuts and seeds (preferably rinsed and soaked to aid digestion), beans that have been soaked, and or sprouted for 48 hours and cooked well, fresh cold water fish, and lean organic poultry.
Bone broth may also be prescribed to help heal and repair the digestive tract and is thought to be effective in treating leaky gut because it is rich in collagen, glutamine and, and gelatin, all helpful nutrients for gut repair.
1 to 2 cups of bone broth may be consumed daily to help repair leaky gut. Bone broth may be made from scratch or bought dry. Here I will sometimes prescribe products like Ancient Nutrition Bone Broth, and have found it quite useful for overall gut health. Usually, when poor digestion improves, emotional changes in the individual are improved as well.
Start With a Good Multivitamin
Additional supplementation usually includes a high-quality multivitamin, preferably hypoallergenic. For women under 40, I usually prescribe Basic Nutrients IV, by Thorne Research, as the best multivitamin on the market. This is because it contains no fillers, and is easy to digest even when digestion has been compromised.
For women over the age of 40, I usually prescribe Meta-Fem—also produced by Thorne Research. Men under 40, may try Basic Nutrients III, by Thorne Research. While men over 40, usually do very well on Al’s Formula by Thorne Research.
Medical Foods To Heal The Gut and Improve Mood
Like many naturopaths, I advise starting the morning with a medical food, that has been specifically formulated to heal poor digestion, and improve mood. This usually means prescribing something like Medi-Clear Plus, by Thorne Research. This product is loaded with good nutrition for gut and brain health, and I usually have patients makes a morning smoothie every day for the first 21-90 days as their digestion repairs itself.
Probiotics To Heal the Gut and The Brain
While there are many good probiotic formulas on the market, I usually prescribe Primal Defense by Garden of Life, and advice the patient take one capsule after breakfast for best results.
If you are suffering from poor digestion, chronic pain and depression, please reach out to me. To find out more about my work, please visit my website at DoctorWhimsy.com. I am available for consultations both in my offices in Los Angeles and by phone and or telemedicine appointment. I look forward to working with you.
Walker, AK Neuroinflammation and Comorbidity of Pain and Depression
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3880465/
Psych. News
https://psychnews.psychiatryonline.org/doi/full/10.1176/appi.pn.2017.pp9b2


transcranial magnetic stimulation west los angeles ca
21 Jun 2020I am really liking this article, thanks for posting!
marketing
26 Jun 2020Do you have a twitter? Can I follow you?